
This February JAMA article is a very large observational study looking at the health risks of taking even very brief courses of therapy with a drug class called NSAID’s. NSAID’s stand for nonsteroidal anti-inflammatory drugs. Here in the US commonly taken products in this category available over the counter include: Motrin, Aleve, naproxen, and ibuprofen. Prescription’s in this drug class include: Mobic, meloxicam, Celebrex, Daypro and many others.
These medications were originally designed to help treat inflammatory arthritis but are taken over the counter for minor aches and pains as well as fever. They are still prescribed for acute joint injuries, acute pain and other inflammatory conditions such as pericarditis, gout or inflammatory arthritis/bursitis.
I have been wanting to review this article for the public because it is a very large data set that mimics the “real world” of health care and medication usage in the United States. If patients and doctors are made aware of this data I think we will find ourselves less “nonchalant” about taking over the counter pain medications.
This past year, popular lay articles and even more recent “scare” health literature about our narcotic/Tylenol (acetaminophen) combination medications Tylenol is significantly safer for minor aches and pains and degenerative arthritis pain. It is true that an acute overdose of Tylenol (acetaminophen) can be fatal. When used properly there is no literature showing nearly the harm from this pain reliever compared to the NSAID class of pills.
This article looked at a specific situation. This situation affects a lot of typical patients and thus this is a “real world” and applicable observational study. It was conducted in Denmark and involved 61,921 patients (that is a large group folks). It occurred from 2002-2011. The study was conducted to look at the safety of using the NSAID’s group of medications in patients who had suffered and survived a recent heart attack. Heart attack patients are recommended to take blood thinners, specifically drugs known as anti-platelet medications.
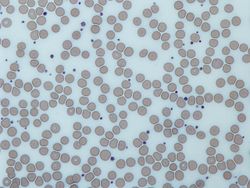
Platelets are noted in this photo above as those tiny “smudges” between the larger cells which are red cells. Platelets can attach to injured endothelial cells and stick to the collagen in the artery wall. These attached platelets then attract other clotting molecules and recruit red cells to cover the injured vessel. If enough clotting occurs the artery well gets blocked with a clot. It the clotted artery feeds heart muscle a heart attack results. This same process in the brain circulation results in a stroke. Studies have proven that in patients who survive a heart attack, taking aspirin or another common anti-platelet medication known as Plavix (clopidogrel is generic name) lowers the odd of a future heart attack. Many heart attack victims have other heart conditions such as a left ventricle aneurysm or abnormal heart rhythm called atrial fibrillation which result in prescribing an anti-coagulant blood thinner known as Coumadin (warfarin is generic). Patients taking these medications for future heart attack and stroke prevention are the group that was analyzed in this particular study.
Now let’s get to the actual study. It was a Danish trial but I feel it can be applied to our US patients. It was an observational trial meaning no intentional intervention was performed, rather data was collected and patients were followed over time. The study occurred over 9 years. All patients observed had been diagnosed and had survived a heart attack 30 days prior to being observed. This eliminated confounding variables of mortality directly related to the first heart attack. There was a 90% liklihood that a real heart attack was the correct diagnosis/condition present in the study group. 34 % of the patients took an NSAID in the study period. All levels of exposure to NSAIDs from as little as 3 days to ongoing past 90 days were counted. The end points looked at included risk of bleeding bad enough to be hospitalized, cardiovascular death and nonfatal heart attack or stroke.
Findings are summarized as follows:
- 18,105 people died (29.2%).
- 5,288 bleeding events occurred.
- 18,566 cardiovascular events occurred (apparently a lot of second heart attacks resulted in death).
- The incidence of bleeding events were nearly double in patients who took NSAIDs with blood thinners. 4.2 per 100 person years versus 2.2 per 100 person years.
- There was a 40% increased risk of cardiovascular events in persons that used NSAIDs with blood thinners.
- There was an increased risk of bleeding and cardiovascular events regardless of antithrombotic medication used if combined with any NSAID.
- The bleeding risk was highest with short duration use (0-30 days).
- The combination of aspirin, plavix and any NSAID had the highest bleeding risk.
- Any combination of aspirin, plavix, warfarin and an NSAID also increased the risk of heart attack or stroke.
I feel patients need to be aware that even a couple of doses of ibuprofen or Aleve over the counter can interfere with recommended blood thinners if you are a heart attack survivor. It is also reasonable to assume that combining these medications even in non heart attack subjects would likely provide similar increased risk. Doctors appropriately recommend aspirin for heart attack prevention before a heart attack and so the opportunity for taking NSAID’s on top of aspirin occurs with a very high rate of occurrence.
Another concern I have as an Internist who provides a lot of coordinated care for adults is that folks who self-refer to other access points especially orthopedic physicians, walk-in clinics and consulting with pharmacists may inadvertently place themselves at unrecognized risk of severe bleeding, hospitalization and even death.